- Long-term survival after CCRT and HAIC followed by ALPPS for hepatocellular carcinoma with portal vein invasion: a case report
-
In-Jung Kim, Sung Hwan Yoo, Jung Il Lee, Kwan Sik Lee, Hyun Woong Lee, Jin Hong Lim
-
J Liver Cancer. 2022;22(1):84-90. Published online March 22, 2022
-
DOI: https://doi.org/10.17998/jlc.2022.03.07
-
-
2,802
Views
-
70
Downloads
-
1
Citation
-
 Abstract Abstract
 PDF PDF
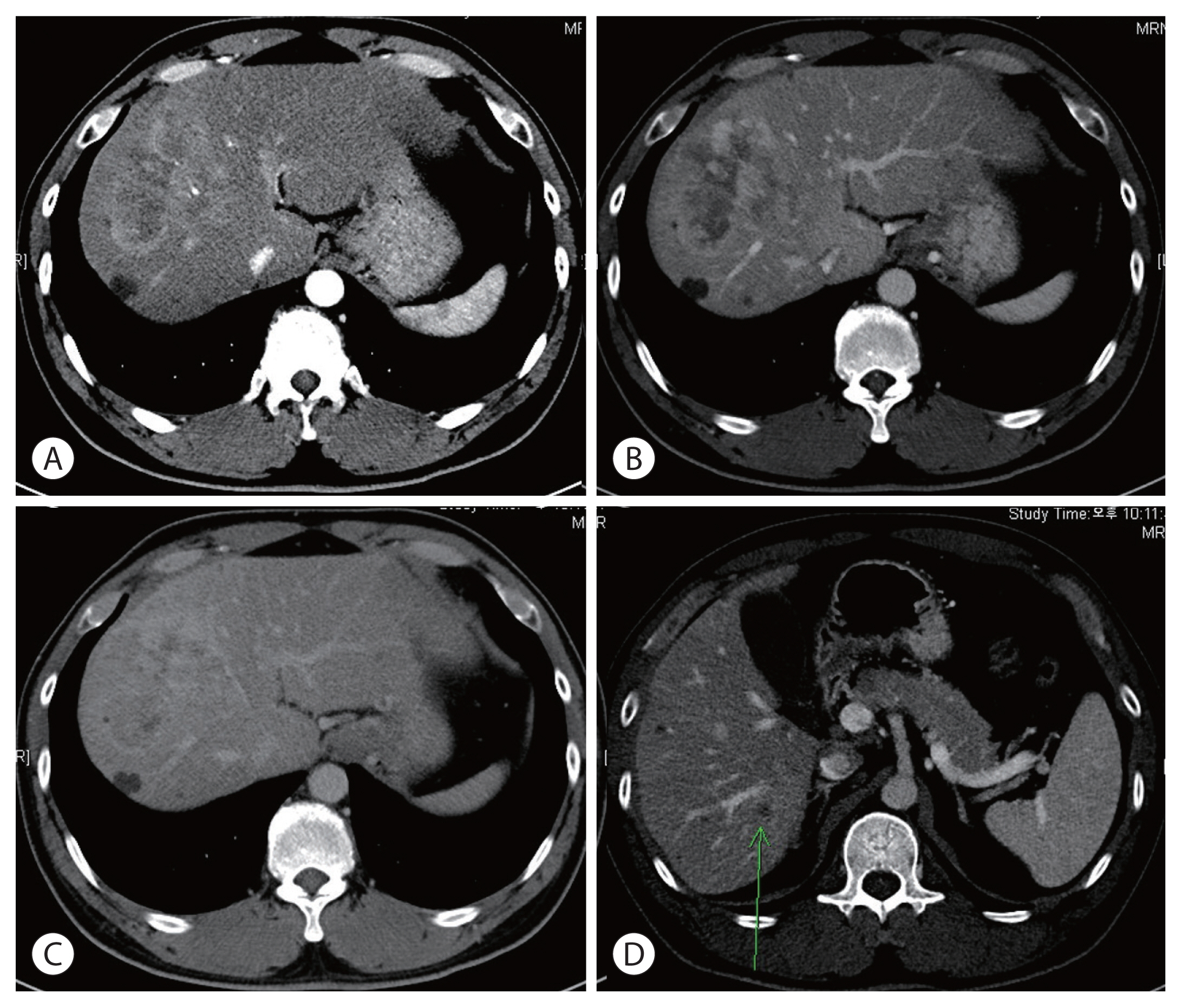
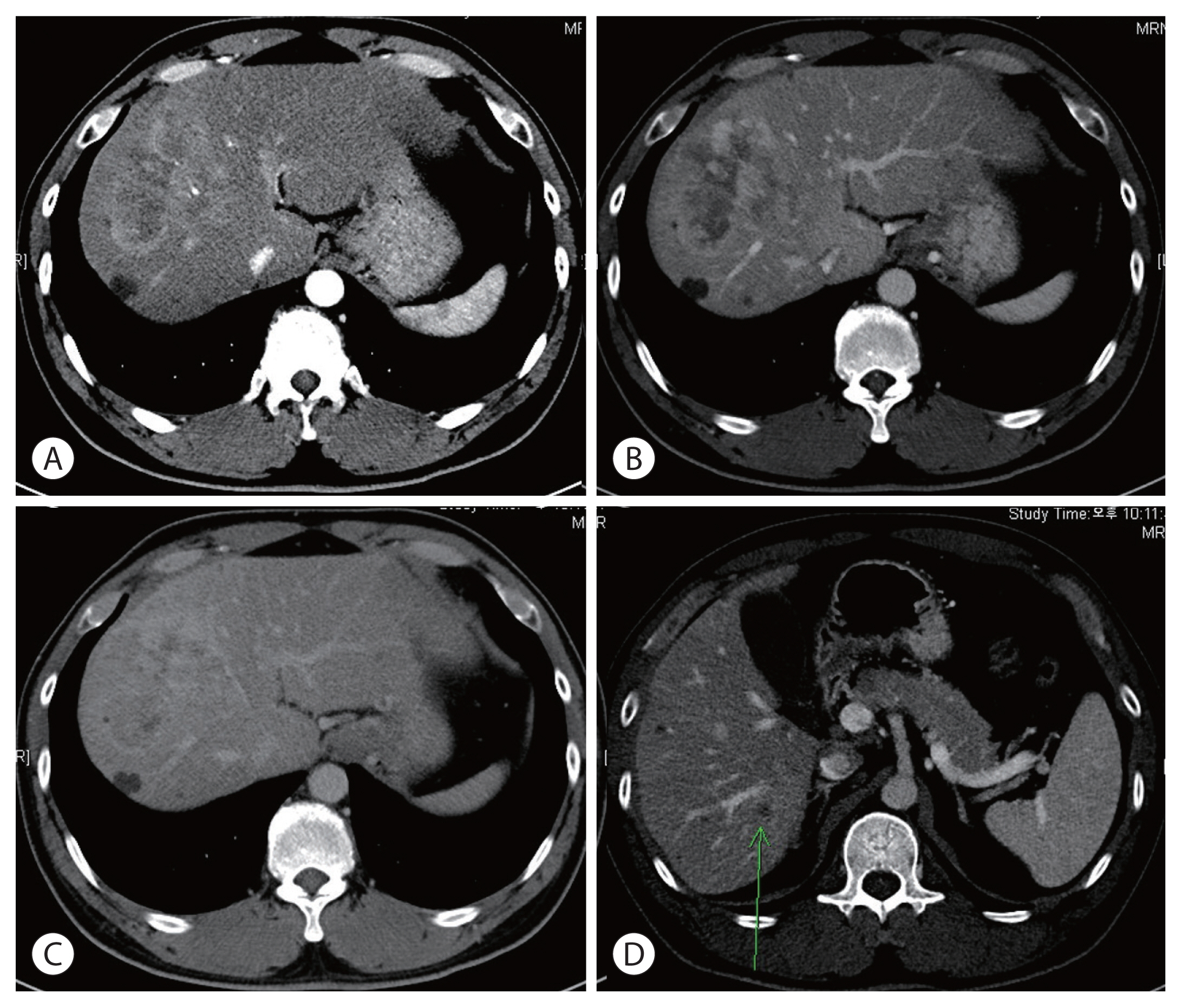
- There are various methods for treating advanced hepatocellular carcinoma with portal vein invasion, such as systemic chemotherapy, transarterial chemoembolization, transarterial radioembolization, and concurrent chemoradiotherapy. These methods have similar clinical efficacy but are designed with a palliative aim. Herein, we report a case that experienced complete remission through “associating liver partition and portal vein ligation for staged hepatectomy (ALPPS)” after concurrent chemoradiotherapy and hepatic artery infusion chemotherapy. In this patient, concurrent chemoradiotherapy and hepatic artery infusion chemotherapy induced substantial tumor shrinkage, and hypertrophy of the nontumor liver was sufficiently induced by portal vein ligation (stage 1 surgery) followed by curative resection (stage 2 surgery). Using this approach, long-term survival with no evidence of recurrence was achieved at 16 months. Therefore, the optimal use of ALPPS requires sufficient consideration in cases of significant hepatocellular carcinoma shrinkage for curative purposes.
-
Citations
Citations to this article as recorded by  - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- A Case of Early and Massive Recurred Hepatocellular Carcinoma in Patients with Ruptured Hepatocellular Carcinoma Underwent Staged-Surgical Resection
-
Sung Hoon Kim, Jin Hong Lim, Sang Hoon Ahn, Kyung Sik Kim
-
Journal of the Korean Liver Cancer Study Group. 2011;11(2):155-159. Published online September 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- The rupture of hepatocellular carcinoma (HCC) has been uncommon complication. Because the diagnosis of early HCC has
been increase due to development of imaging modality and surveillance program, the incidence of ruptured HCC has
been decreased. The paradigm of treatment for ruptured HCC has shifted from surgical hemostasis to transcatheteric
chemoembolization (TACE) at acute phase. After the control of acute phase, the definitive treatment for HCC is still debate.
However, many studies have advocated staged-liver resection. Some studies reported that the patients underwent staged-liver
resection showed a similar survival rate compared with survival rate in patient with non-ruptured HCC. The staged-liver
resection was usually performed in the patients with well-preserved liver function. The decision of optimal time for surgery after
TACE and surgical indications for ruptured HCC after any other primary treatment are controversy. We experienced a cases of
early and massive recurrence HCC in patients with well-preserved liver function and the rupture of HCC. The further study may
be needed to decide the optimal time of surgery after TACE and surgical indication for rutprued-HCC.
- A Case of Concurrent Liver Resection and Splenectomy in Patients with Hepatocellular Carcinoma and Decompensated Liver Cirrhosis
-
Sung Hoon Kim, JIn Hong Lim, Sang Hoon Ahn, Kyung Sik Kim
-
Journal of the Korean Liver Cancer Study Group. 2011;11(2):160-164. Published online September 30, 2011
-
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma (HCC) develops on chronic liver disease and often accompanies portal hyperternsion. Portal
hypertension induces hypersplenism with splenomegaly. Because hypersplenism results in pancytopenia, especially
thrombocytopenia, it is not easy to decide the hepatic resection for many surgeons in patients with HCC and hypersplenism.
Although liver transplantation is the most ideal treatment for HCC and hypersplenism, liver resection has been performed
commonly because of donor shortage. Splenectomy has performed to control intractable varices as a Hassab’s operation
(=decongestion of upper gastric marginal veins and splenectomy). Recently, as a development of surgical techniques and
equipments, especially laparoscopic surgery, splenectomy has been performed safely and easily. Some studies reported that
splenectomy improved the liver function. Splenectomy in patients with HCC expanded the indication of liver resection and
increased disease free survival (DFS). However, portal vein thrombosis (PVT) is a one of well-recognized complications of
splenectomy and recent prospective study reported the 50% rate of PVT in non-cirrhotic splenectomized patients. Some studies
reported that splenectomy with simultaneously or staged liver resection was performed safely without a significant complication
and operative mortality. We experienced a case that underwent simultaneously liver resection and splenectomy and then
recovered without complication. The further study may be needed to evaluate the role of splenectomy in patients with HCC and
hypersplenism.
|